Beyond Clinical Practice: Why Doctors Are Moving into Health Information Management & CDI
Healthcare is changing day by day. The doctors are now working on automatic healthcare systems and AI tools on an everyday basis. These tools make the work organised in hospitals, but they also create pressures like more screen time, a lot of documentation, and the doctors feel more burned out. Because of all these difficulties, the doctors are now planning for a medical coding certification and looking for new jobs that give them stability, less stress, and keep them connected to the healthcare system.
This is where the Health Information Management (HIM) comes into the picture. This is not just a backend job. It is an important part of the operations that are done in the hospitals. This HIM combines data management and digital systems and is one of the most important systems in the hospital.
Hospitals are mostly dependent on accurate data, and it is important for them to have people who can connect clinical knowledge with the digital systems. Doctors are the people who fit best in this role because they are good at making decisions, they are aware of patient care, and they also know every medical term.
Why Doctors are Irreplaceable in Health Informatics Systems
One of the biggest problems in hospitals today is that many Health Information Systems, whether it’s Oracle Cerner, Meditech, Epic, or Allscripts, are not built around clinical workflows. They are supposed to support end-to-end care, from registration to billing, but let’s be honest, sometimes the system feels slow, complicated, and disconnected from the way things actually happen in the wards.
But doctors bring clinical insights and on-ground experience that no software engineer or data specialist can fully replicate. This is because they understand what happens in real patient care: how diagnoses are made, what workflows in hospital wards are, and what information really matters for treatment. Doctors can help design and tailor the digital systems to support real-world patient care.
When physicians step into Health Informatics roles like CMIO or physician informatics, they become important as they bridge between IT teams, administrators, and clinicians. And this helps in ensuring EHRs, decision-support tools, and digital workflows are designed around real clinical needs by improving safety and usability.
Should a Doctor get a Medical Coding Certification?
If you’re a doctor wondering whether you should get a medical coding certification, the answer is: it depends on what you want out of your career.
In the healthcare industry, the diagnoses, procedures, and treatments are translated through the technical skill called medical coding. They do this by using standardized codes like CPT and ICD-10.
Medical coding is a technical skill in which professionals translate diagnoses, procedures, and treatments into standardized codes such as ICD-10 and CPT.
It is essential for billing, insurance claims, and proper documentation, and there is a growing demand for skilled coders, according to sources like Coursera and Goodwin University.
If you are a good doctor, it does not mean that you can eventually be a good coder. According to the data, when doctors try to code on their own, the error rate is surprisingly high; some analyses report rates as high as 60%.
The reason is that coding requires detailed, instruction-driven work, whereas doctors are trained to focus on patient care. Also, coding can be time-consuming. Most doctors already feel overwhelmed with their clinical duties, and adding coding to that workload is not feasible.
For doctors, medical coding certification is not the final goal. It is the entry permit to something more impactful: Clinical Documentation Improvement (CDI). CDI ensures that what’s written in the patient chart truly reflects their real condition–every symptom, diagnosis, decision, and outcome.
This directly impacts patient care, hospital revenue, and compliance audits. And here’s the truth: only a doctor has the clinical judgement to question or guide another doctor’s documentation. That’s why hospitals often prefer doctors/physicians, especially those who understand coding, to lead or support CDI programs.
How Medical Coding Can Help Doctors
When a doctor decides to get a medical coding certification, it can actually help in more ways. When they are certified in medical coding, they learn to translate clinical diagnoses and procedures into standardized codes such as ICD-10, CPT, and DRG.
Usually, for a smooth reimbursement process, good documentation and billing skills are necessary. And the doctors can ensure these very well. And just to be clear, this isn’t about becoming a full-time coder.
The purpose of these skills is to give various opportunities to different roles, like CDI, roles in auditing, and positions that require documentation skills. Here, the doctors play well because their good clinical judgments make a huge difference.
Most physicians start with a simple coding certification, such as the CPC or CRC. These give you the foundational knowledge you need– how coding rules work, how proper documentation should be, and how diagnoses and procedures are classified. But this is just the first step. Once they understand the basics of coding, it makes sense to move on to advanced credentials like CCDS or CDIP.
Medical coding can also help doctors in their own clinics; they don’t have to rely on someone else for billing and documentation.
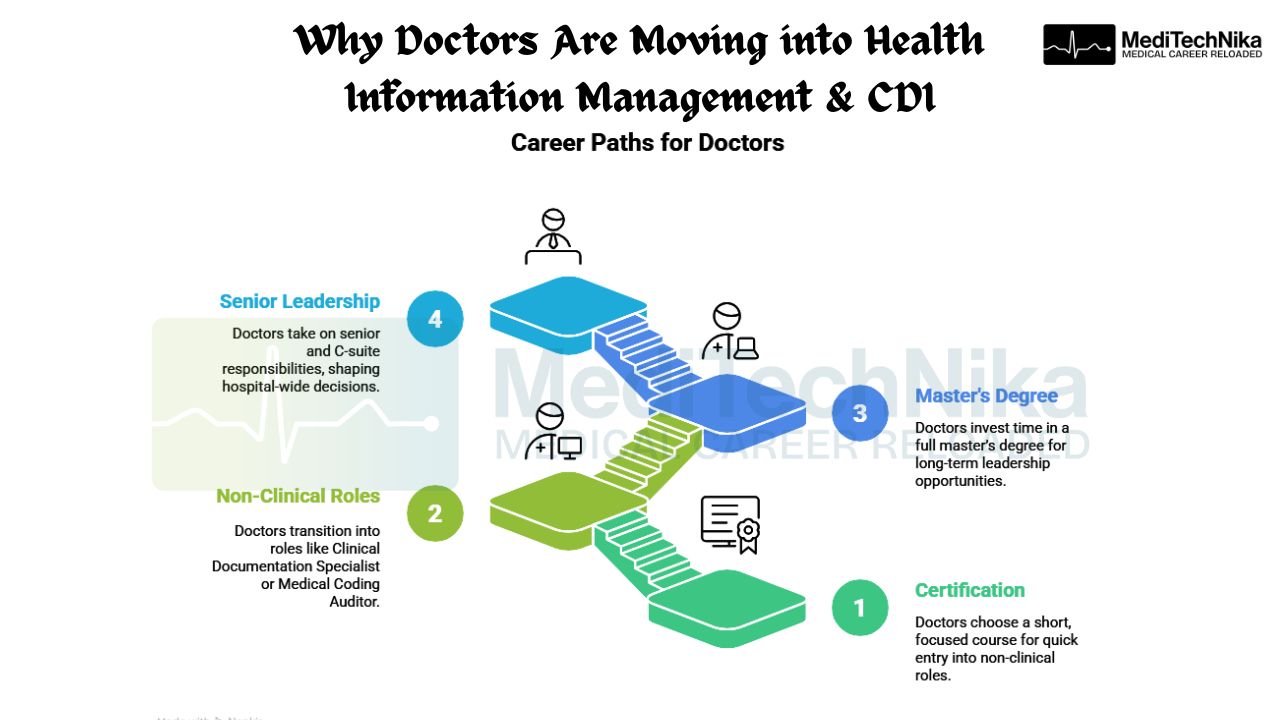
Which path to choose: Degree vs Certification
While pursuing the degree, choosing between the degree and certifications becomes a tough decision. But if you are clear about your path, goal, and the time in which you want to achieve it, then it becomes easier. If you are planning to work in the industry a little sooner, then getting a certification is the best option.
There are a few certification courses, like AAPC and AHIMA, that take only a few months to finish. This is because these courses are designed to teach them what is required for the industry. They teach coding with applications like CPT, HCPCS, ICD, documentation rules, and guidelines for billing.
If you are someone who is planning to take a break after residency, then getting a certification is the right choice for you. It is also better for people to earn more while they are practicing.
A degree, on the other hand, gives you a much wider foundation, and programs in Health Information Management typically take longer: 2 to 4 years, but they cover everything. According to the internet data, degree holders tend to qualify for more roles, such as health information management, auditing, EHR administration, and even supervisory positions. They also tend to have higher long-term earning potential.
Doctors are Shaping the Future of Healthcare Data
There are so many healthcare systems in the world that are trying to find people who understand clinical work and digital health tools, and that is why doctors who learn medical coding, HIM, or CDI are in demand. But there are not many professionals who know both things, so this opens huge opportunities for the physicians right now.
The doctors bring the clinical thought and thinking together through the data. And they do this by learning coding. Doctors are the best people to understand complex information, spot different trends, and guide changes that benefit patients.
In the coming years, hospitals will rely heavily on doctors to help keep their data accurate and well-managed. Good documentation not only keeps data organised, but it also directly affects how hospitals get paid.
As healthcare becomes more data-driven, doctors who step up as data-proficient individuals are likely to shape the future of medicine by making it smarter, safer, and more responsive to what patients actually need. Since doctors understand both the clinical and technical sides, they naturally become the link between IT and clinical staff. And when they help improve documentation, patient care benefits as well.
Keynote
When we look at where healthcare is headed, it is clear that doctors who understand Health Information Management, medical coding, and CDI will be the real game-changers. And as the global reports suggest, the need for professionals who can bridge clinical knowledge with data, analytics, and technology is growing every year. We know not everyone can fill the gap. Doctors already have the clinical expertise and the ability to understand the reason behind every scan and treatment. When doctors combine their knowledge with HIM, we can see that healthcare and technology come together.
This path also offers stability, work-life balance, and long-term career growth without pushing doctors away from the world of medicine. Whether the doctor chooses an advanced CDI credential certification or a HIM degree, it takes them closer to the roles where medical judgment matters as much as technical understanding.
We believe the future of healthcare needs doctors who can do clinical and digital both. This will create a huge difference in the healthcare industry if more doctors come forward to learn.